Radical radiotherapy is another treatment for prostate cancer. It is suitable for men of any age and is an effective alternative to surgery. The aims of radiotherapy are to destroy prostate cancer cells and to stop them from growing. Here we cover the different types of radiotherapy and the potential side effects.
Radical Radiotherapy
What is involved and what are the risks?
You can receive radiotherapy in one of two ways:
• External beam radiotherapy High energy X-ray beams aimed at the prostate from outside the body.
• Brachytherapy Small radioactive sources positioned inside the prostate. There are two types of brachytherapy that can be used for different stages of prostate cancer.
Who are these treatments suitable for?
As with surgery, radical radiotherapy is recommended for men with a good life expectancy. It is an alternative for men whose cancer can be treated radically, but who are not fit enough or choose not to have an operation.
Radiotherapy does not have the same risks that are associated with surgery, such as blood clots or blood loss. You will not have to stay in hospital during the therapy and many men are able to continue with their normal daily activities. However, it is not a ‘softer option’ – it carries its own risks and side effects, which you must consider before making this choice.
External Beam Radiotherapy
External beam radiotherapy is used to treat prostate cancer by aiming beams of high-energy X-rays at the prostate gland and the tissues immediately around it. The X-rays damage cells and stop them from growing. Cancer cells are not able to recover from this damage, but the cells in the normal tissues surrounding the prostate (bladder and bowel) can repair themselves more easily. It can be used in conjunction with chemotherapy or used before surgery (neo-adjuvant radiotherapy) or used after surgery (adjuvant radiotherapy), in order to make those treatments more effective.

The first step in external beam radiotherapy is to have a special planning scan (CT scan) of your pelvis. This is done to see exactly where in the prostate the cancer is and whether it has spread to areas around the prostate gland or other parts of your body. The information on this scan will allow your doctor (oncologist) to see exactly where your prostate is and map the areas that need treatment.
During the scan the doctor will place small, permanent marks (dots the size of a freckle) of ink onto your skin. These permanent ‘dots’ will be used to ensure that the exact same area is treated for each of your treatment sessions.
The doctor may ask a radiotherapy physicist to make an individual plan for your treatment. They will use a computer program to decide exactly where the X-rays need to be aimed to treat your prostate gland while trying to avoid as much of the normal tissue in the surrounding areas (bowel, bladder) as possible. This process is very complicated and can take up to a few weeks to be completed.
When the doctor is satisfied with your plan, you may need to go back to the radiotherapy department for one further visit for a final check to position the X-ray beams before the actual treatment starts. (This is known as a verification visit.)
The X-rays are made in a special machine called a ‘linear accelerator’. When you go for treatment, the radiographer will ask you to lie on your back on a firm bed attached to the machine. Part of the machine will move around you and direct X-rays at your prostate from different directions.
The treatment will only take a few minutes and is completely painless. It is important that you lie very still while the treatment is being given. You may be asked to drink some water before each therapy as this will fill your bladder and reduce the amount of bladder tissue in the radiotherapy beam.
You can expect to have between 20 and 40 treatment sessions over four to eight weeks as an outpatient from Monday to Friday (not weekends).
There are two main types of external beam radiotherapy that are available and these use different methods to reduce the amount of radiation given to the normal tissues surrounding the prostate gland. This can reduce side effects and also allow higher doses of radiation to be concentrated on the prostate gland itself.
3D conformal radiotherapy (3D-CRT)
3D-CRT uses special ‘blocks’ within the linear accelerator to shape the beams to fit the exact shape and size of your prostate.
Intensity modulated radiotherapy (IMRT)
IMRT uses a computer-driven machine that moves around you as it delivers the radiation. It can be used to adjust the dose of radiotherapy given to different parts of the treatment area, which can then limit doses of radiation reaching nearby normal tissues. Your doctor may recommend that you take a course of hormone therapy before radiotherapy to shrink the prostate, and maybe afterwards for some months.
Other Types of External Beam Therapy
Image-guided radiotherapy (IGRT)
IGRT is usually done alongside IMRT. With IGRT, images are taken before or during radiotherapy that show the size, shape and location of the tumour to allow the doctor to make minor adjustments in aiming. This helps to deliver the radiation even more precisely and results in fewer side effects.
Stereotactic body radioation therapy (SBRT)
SBRT uses advanced image-guided techniques to provide large doses of radiation to a precise area. Since there are large doses of radiation in each dose, the entire course of treatment is given over a few days. SBRT is often known by the trade names of the machines that deliver the radiation, such as Gamma Knife and CyberKnife. There are other forms of external beam radiotherapy available as part of clinical trials.
Brachytherapy
This form of radiotherapy can be given in two ways:
● low-dose-rate (LDR) permanent seed brachytherapy; or
● high-dose-rate rate (HDR) temporary brachytherapy.
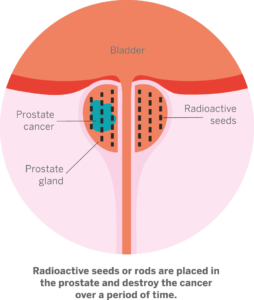
Low-dose-rate (LDR) permanent seed brachytherapy
This is an effective treatment for some men with early prostate cancer and uses radioactive seeds. It can also be effective for some immediate or high-risk patients. You will be carefully assessed before treatment to make sure that your prostate is not too big as this treatment can cause difficulties with passing urine if the prostate is very enlarged.
The seeds are placed in the prostate in in the prostate through the skin of the perineum (the area between the anus and scrotum). You will need an anaesthetic for this procedure. However, the needles are withdrawn and the seeds are left permanently inside the prostate where they slowly lose their radioactivity with time and treat the prostate cancer.
Although the seeds are radioactive, you are not. As there are low levels of radiation in the seeds, as a precaution you may be asked to avoid close contact with pregnant women and young children for at least two months after the treatment. This treatment can be a quicker alternative for some of the men who cannot visit a radiotherapy centre each day.
This treatment has similar side effects to external beam radiotherapy but the risk of urinary problems is slightly higher and the risk of bowel problems is slightly lower in brachytherapy.
High-dose-rate (HDR) temporary brachytherapy
This treatment can be used as well as external beam treatment to allow a higher dose of radiation to be given to the prostate and surrounding tissues for men with locally advanced or high-risk prostate cancer.
Hollow rods or needles are placed in the prostate through the skin of the perineum (the area between the anus and scrotum). You will need an anaesthetic for this procedure. After the needles have been placed, you will have a scan (CT or ultrasound scan) to check their exact position and your doctor and a physicist will use this information to plan your treatment.
The needles will stay in your prostate until the treatment has finished, during which time you will need to lie on your back and a catheter will be placed in the bladder to help you pass urine. A small radioactive pellet is put in each rod for a few minutes. You will be given the precise dose of radiotherapy that you need based on your treatment plan. The radioactive pellets are then removed after each treatment. Once the radioactive pellets are removed, you will not give off radiation or be radioactive.
You will stay in hospital for a few days until you can pass urine normally after the catheter has been removed. You may have a shorter course of external beam radiotherapy (four to five weeks) two weeks after the brachytherapy treatment. The side effects are similar to those from external beam radiotherapy apart from a small extra risk of developing a narrowing of the urethra (stricture) – likely for about one in every 20 men.
What happens after radiotherapy?
You will be seen in the outpatient clinic a few weeks after the radiotherapy finishes and regularly for many years afterwards for follow-up appointments.
Your follow up appointments will usually start two or three months after treatment. Your PSA will be checked and you will be asked about any side effects from the radiotherapy treatment. You will be given the chance to discuss any questions or concerns.
If your treatment has been successful, your PSA level should fall which can take many months. if you are also being treated with hormone therapy, the hormone therapy will also reduce the PSA level. You will still have a measurable PSA level because you still have a prostate gland and the normal prostate cells will produce a small amount of PSA.
After radiotherapy, some men experience what is known as a PSA bounce, in which the PSA rises for a short time within the first couple of years after treatment, but then goes back down. Doctors aren’t sure why this happens, but it doesn’t seem to affect your prognosis.
If your first treatment option was radiation therapy, and the cancer comes back, your other treatment options may include radical prostatectomy, which is the removal of your prostate gland and surrounding tissues.
Acute or short-term side effects of radiotherapy
These are temporary and usually happen in the last two to three weeks of treatment and start to improve a few weeks after the treatment is over.
Sore skin You may experience some darkening, redness and/or soreness of the skin in the area being treated. This is most common in the skin between the legs and around the anus. You should avoid using any creams, lotions or soaps, unless recommended by your doctor, and also avoid hot baths. You may also lose some pubic hair in the area being treated but this will usually grow back.
Bowel changes You may develop some discomfort and pain in the back passage (rectum) and this can be worse when you go to the toilet to open your bowels. This is called proctitis and can be treated with creams and suppositories.
Many men find that their bowel movements become loose and more urgent as the treatment progresses (diarrhoea).
You may also notice a little leakage from the back passage and occasionally some blood or mucous (slime) in the stools. You will be given advice about diet and medication if diarrhoea becomes a problem. The diarrhoea should gradually get better a few weeks after your treatment. However, let your doctor know if it continues.
Some men experience radiation enteropathy, which is inflammation of the intestines after radiation therapy. It can take place early on (acute) when it occurs within three months of radiation therapy, or it can be delayed (chronic) when it occurs between 18 months and six years after radiation therapy. You may experience symptoms such as diarrhoea, nausea, vomiting and stomach cramps. Talk to your doctor if you are experiencing any of these symptoms, as they may recommend changes to your diet and medication.
Bladder changes You may have to pass urine more frequently both during the day and at night. Your urine stream may slow down and you may feel a burning sensation (radiation cystitis) when you pass urine. Owing to the weakening of the blood vessels in your bladder and bowels, you may also notice blood in your urine. If you notice any bleeding in your urine and bowels, always tell your doctor so they can check it out.
Feeling tired Towards the end of treatment and for a few weeks after, you may feel more tired than usual.
Being sick or feeling sick There may be times that you feel sick. You can take anti-sickness medicines. If you still feel sick after that, let your treatment team know.
Permanent or long-term side effects of radiotherapy
Most side effects go away after treatment, however, some continue for many months, come back, or develop years later (these are called late effects). The following side effects can happen after the radiotherapy has finished.
Bowel changes Between one and five men in every 100 will have some long-term bowel changes. These can include diarrhoea or urgency to open your bowels (radiation proctitis), minor bleeding or some mucous from the rectum when passing a motion.
Bladder changes A small number of men may find it more difficult to pass urine. This difficulty will be a gradual process that occurs over a few weeks or months, and is due to the narrowing of the tube from the bladder to the penis (the urethra). Tell your doctor if you have trouble passing urine. About 5% of men have moderate to severe problems with leaking urine six years after their treatment ends. If this happens, speak to your doctor as they may be able to refer you to a specialist incontinence clinic.
Sexual changes About 50% of men will have problems getting an erection after radiotherapy. The risk may increase if you have also been treated with hormone therapy. Treatments may be available to help. Radiotherapy may also cause you to produce less semen and reduce your sperm count, which may lead to infertility. Some men may find this difficult to cope with. If you are worried, talk to your doctor, as you may be able to store sperm before treatment starts.
Dry orgasm This is when you feel the sensation of orgasm but you do not ejaculate. You could also experience retrograde ejaculation, which is when there is a delay, and semen comes out after you orgasm.
Swollen legs or scrotum Some men experience swelling (known as lymphodoema) in their legs or the sack of skin around the testicles (the scrotum), which can be uncomfortable. This happens because the lymph channels that drain fluid from the legs are damaged by the radiotherapy.