Reducing barriers to screening in Black men with prostate cancer
Project Summary
About the Researchers
Dr Hari Iyer
Principal Investigator
Hari is Assistant Professor at Rutgers Cancer Institute of New Jersey and his research examines multilevel environmental, health care access, lifestyle and biological pathways that drive risk of prostate cancer.
Professor Timothy Rebbeck
Principal Investigator
Timothy is the Vincent L. Gregory, Jr. Professor of Cancer Prevention at the Harvard T.H. Chan School of Public Health and Dana Farber Cancer Institute. He studies the etiology and prevention of cancer, with an emphasis on cancer disparities and global health.
The gap
Racial disparities among men with prostate cancer are among the largest for any common cancer.
In the United States, Black men are more likely to develop, die, and be diagnosed at an earlier age than other men. Approximately 1 in 4 Black men will be diagnosed with prostate cancer compared with 1 in 8 White men, and it is estimated that Black men are 2.2 times more likely to die from prostate cancer each year.
Black men have the highest mortality rate for prostate cancer of any race and ethnic group in the United States. In comparison to the rest of the world, Black men in the US and Caribbean have the highest documented prostate cancer incidence rates.
1 in 4 Black men will be diagnosed with
prostate cancer
Once the findings are reviewed, Hari and Timothy will talk to health care professionals and community leaders who will help vulnerable populations and neighbourhoods understand and access screenings for prostate cancer.
Racial inequity in prostate cancer screenings
Prostate cancer screening is controversial, and differences in attendance rates can be caused by racial and social disparities.
Black men are often less likely to be able to access prostate cancer services compared to White men. But, in studies where Black and White men have equal access to prostate cancer care, there are fewer differences in prostate cancer specific mortality, suggesting that delivery of proper prostate cancer screening could help to reduce these disparities.
Not enough studies have focused on the differences in treating Black men and White men with prostate cancer, and why Black men have a higher mortality rate. Few studies have examined the links between genetics and biology in Black and White men with prostate cancer, but even fewer have investigated barriers to neighbourhood factors and prostate cancer screenings.
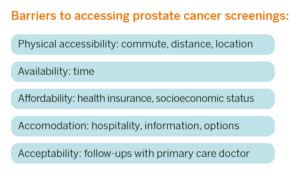
We know that Black men disproportionately face barriers accessing PSA screening, but few studies have examined links between neighbourhood factors, barriers to PSA screening access, and prostate cancer mortality.
The results will be made available to patients and families through a web-based portal to examine trends in prostate cancer and how they apply to the individual patient based on location.
The research project
Hari and Timothy will use data from across the US to estimate the impact of geographically targeted interventions to eliminate barriers to access prostate cancer screenings.
Important barriers to accessing screenings to predict prostate cancer specific mortality vary by individual and neighbourhood level factors. To remove the barriers relevant to individual and neighbourhood context, policies must be created and implemented to increase access to prostate cancer screening in vulnerable communities.
Hari and Timothy will use data from across the United States to determine what socioeconomic, neighbourhood, and environmental factors must be removed or changed to eliminate barriers to accessing screenings and treatments for prostate cancer; thereby reducing mortality rates in Black men.
The project uses a technique called geospatial analysis to identify people and places experiencing excess mortality from prostate cancer and their limited access to screenings.
Geospatial analysis is the gathering, display, and manipulation of imagery data provided from GPS satellites to provide insight into relationships between factors and reveal patterns and trends.
Using geospatial analysis, the researchers will model ideal conditions and remove barriers to PSA screenings. Then they will compare and evaluate the effects of the interventions.
Patients and their families will be able to be a lot more involved and proactive when it comes to accessing prostate cancer screenings, asking doctors the right questions, and spreading awareness in the community.
“Using nation-wide cancer registry and patient survey databases will allow us to identify generalizable predictors of screening use and survival, while also allowing us to dig deeper into the local neighborhood, behavioral, and sociodemographic characteristics that influence access and risk of prostate cancer in Black men. Study findings will inform the development of equity-oriented health care delivery interventions to reduce excess mortality among Black men with prostate cancer.
Dr Hari Iyer and Prof Timothy Rebbeck
Lead researchers